This partnership utilizes an artificial intelligence model created by Carebot. With its help, radiologists can detect even difficult-to-recognize tumors, enabling earlier patient care. Business development manager Marek Šťastný participates in this collaboration within BMS. He appreciates the benefits of artificial intelligence in healthcare; according to him, AI can significantly help overburdened doctors. How does Carebot’s technology work? How many hospitals are currently using it? What will be the future of AI in healthcare? Read the interview with Marek Šťastný. The results of the project were presented at the Prague.bio Conference 2025.
How did the collaboration between Bristol Myers Squibb and Carebot on improving early detection of lung cancer come about?
At the beginning of 2022, I reached out to Dan Kvak and Matěj Misař from Carebot. I was intrigued by their project that helped doctors recognize pneumonia in COVID patients. That’s when we first started talking about the possibility of using their AI to detect early stages of lung cancer. It occurred to me that Carebot’s software could help with this disease, which kills more people in the Czech Republic than any other. After ten years of working with lung cancer patients, one feels a certain frustration. About 6,500 new cases are diagnosed here each year, and approximately 75% of them die within a year. The main reason is that most patients (60-70%) only see a doctor when they have an advanced tumor that can no longer be operated on. These patients then have a very poor prognosis.
At the same time, new findings about immunotherapy emerged, which significantly improves treatment outcomes in early stages of cancer. The discovery of so-called checkpoint inhibitors represented a breakthrough in oncology. Their discoverers, Jim Allison and Tasuku Honjo, received the Nobel Prize in Physiology or Medicine in 2018 for it. Data from late 2021 showed that immunotherapy can fundamentally improve the prognosis for early stages of lung carcinoma.
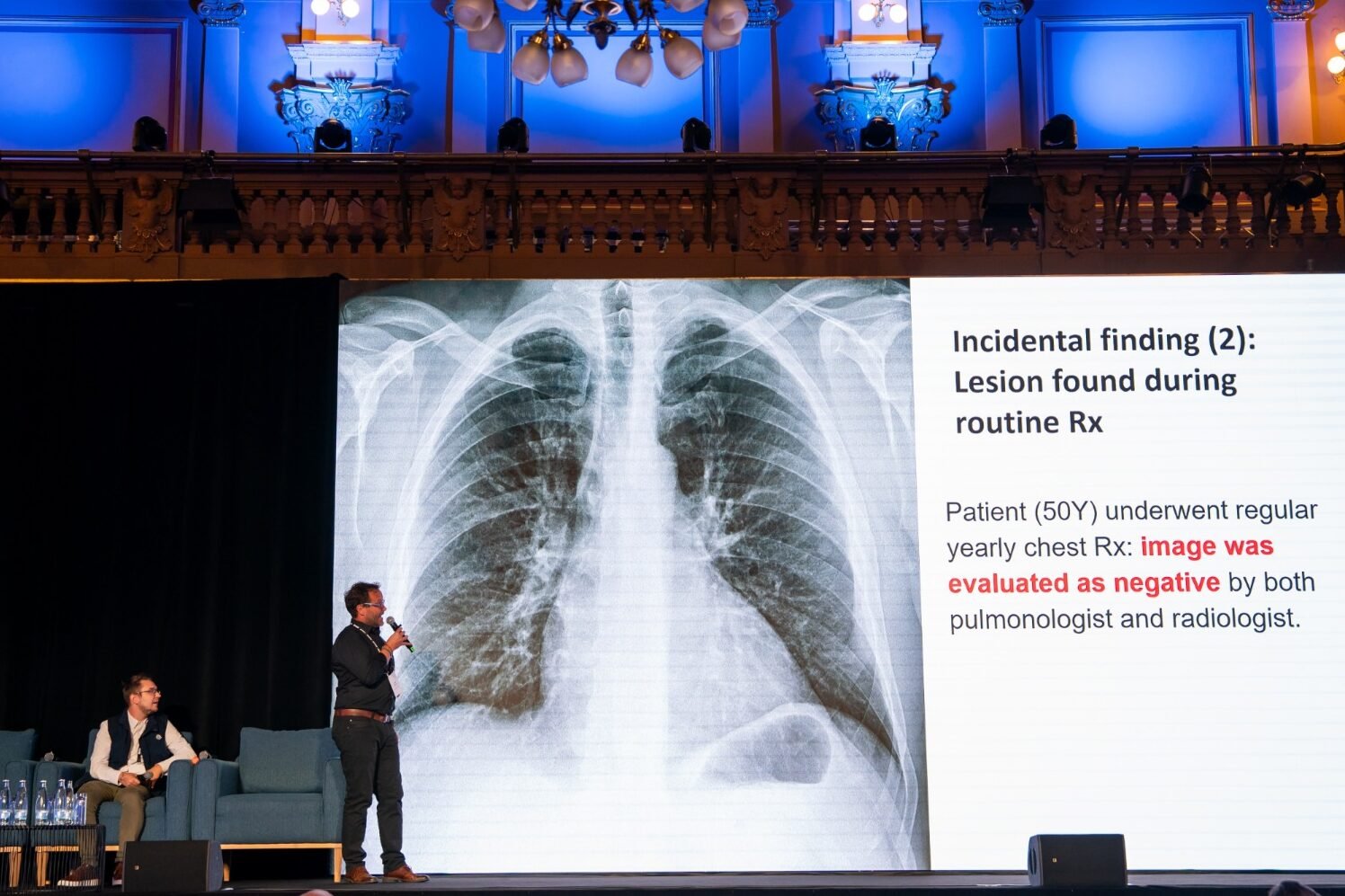
Our thinking was that early detection using AI and the Carebot application could increase the number of patients discovered „accidentally“ and, most importantly, early. During routine check-ups or when patients come for chest X-rays for reasons other than breathing problems.
What goals does this collaboration set?
The collaboration and support from BMS is focused specifically on early diagnosis of pulmonary abnormalities. Carebot operates mainly in smaller hospitals, where it can catch suspicious findings and direct patients to large university facilities. There, specialists can perform further examinations, possibly surgery and modern treatment – including so-called neoadjuvant immunotherapy, where the patient undergoes treatment before the procedure.
At this stage, immunotherapy has the greatest effect. The tumor is smaller, less mutated, and has fewer so-called resistant cells. Some patients can therefore have long-term benefit from treatment. This activity nicely complements the Low Dose CT screening project for detecting lung carcinoma in at-risk patients aged 55 to 74.
What do you see as the biggest benefit of Carebot’s AI solution for clinical practice?
The main benefit is early detection of tumors across the entire population. Carebot’s technology can be used in evaluating up to three million chest X-rays, which are taken in the Czech Republic every year. And the number of lung scans performed is constantly growing, while the number of doctors remains more or less constant.
How many hospitals in the Czech Republic (or abroad) are now involved in the pilot project as of fall 2025? What is their feedback?
Currently, seven regional and two university hospitals are participating in the project. AI mainly helps doctors who have less experience interpreting images. The risk that they will overlook a small finding is higher. Radiologists therefore welcome AI’s help; Carebot serves as a useful assistant to them.
Can it be statistically quantified how AI involvement will reduce the number of lung cancer deaths?
It’s difficult at the moment. However, we have data from the Low Dose CT project from the USA, the Netherlands, and Belgium. Those projects targeted at-risk smoker patients in the age group over 55. The Low Dose CT program reduced lung cancer mortality by 20% in the USA and by 24-30% in both European countries. We don’t have Czech data yet; they will be available next year. But we already know that Carebot has detected overlooked lesions and in some cases caught the tumor earlier.
We consider the project successful not only in the USA but also in Europe. It has great resonance within BMS and will soon expand to other European countries as well. It’s an excellent calling card for the Czech team and a great credit to general director Karin Bacmaňáková, who pushed the project through and secured its funding.
Can AI today offer something in diagnostics that is difficult for doctors to detect?
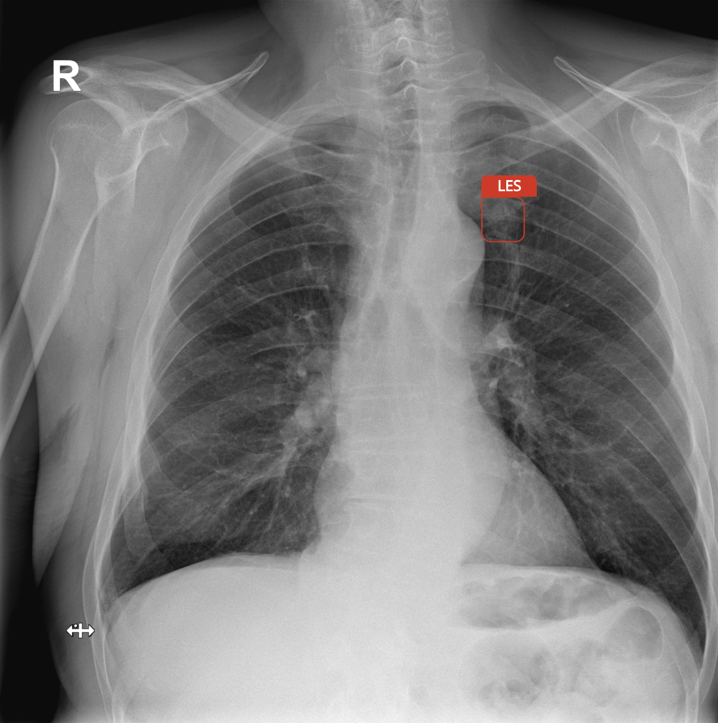
Yes. The human eye has its limits, while AI can detect even small lesions that may be hidden between ribs or near the collarbone. Good training of the AI model and properly set algorithms can recognize subtle changes in lung tissue structure that may indicate a risky abnormality. AI can sometimes detect even tiny textures that are difficult to recognize with the naked eye. And yet these changes may be related to a tumor lesion or other pulmonary disorder.
How do you perceive the role of AI in imaging methods – is it more of a supplement or a future standard?
For now, AI is a smart assistant, but in the future it will probably become a common standard. If it maintains high accuracy and doesn’t produce an excessive number of false findings, it can significantly ease the work of radiologists.
Carebot’s results from Czech practice have shown higher accuracy and almost the same number of false positive results. AI also speeds up image description and makes diagnostics more precise. The advantage is that it doesn’t get tired and, when properly trained, helps reduce the number of errors. If detection algorithms are properly set, then AI should definitely help with early detection.
What requirements does the integration of AI in cancer detection place on doctors? Do they need additional education?
Radiologists don’t need to retrain because of AI. Carebot works very intuitively and serves as a „third eye.“ It marks suspicious spots, but the final decision is always made by the doctor.
The process doesn’t disrupt the normal workflow. Carebot’s system evaluates the captured image in real time, without any intervention from doctors, within just a few seconds.
What are the biggest obstacles that currently prevent faster deployment of AI systems in healthcare?
The biggest concern is the risk of too frequent false positives – that is, marking harmless changes as suspicious – for example, benign pulmonary nodules, lung scars, or old lesions from pneumonia, tuberculosis, and other diseases. Radiologists are concerned that this could lead to system overload and unnecessary examinations.
High-quality AI training on a broad sample of images is therefore crucial. The well-known rule „garbage in – garbage out“ applies. If the data isn’t sufficiently representative, the system may overlook certain types of lesions.
To illustrate, Carebot recently marked a „suspicious lesion“ that was shaped like a shark. It turned out that the patient had a badge with this fish pinned to their shirt. The AI naturally had no idea it was a decoration – it evaluated the shape based on what it knew. This is another example of why AI methods are only a supplement or aid in tumor diagnosis and the final decision must always be with the doctor.
What are the biggest changes AI will bring in the near future in oncology?
The use of AI in healthcare is enormous, and the question is not whether but when. AI will enable identification of new molecules almost in real time and identify potential drugs that have the greatest chance of succeeding in clinical trials. Currently, tests are underway for AI applications that can estimate the outcome of phase III clinical trials within three weeks instead of three years (which is the typical duration of a clinical trial). There are also AI models that can predict with up to 90% accuracy whether a certain abnormality will develop into a tumor within three to five years.
Another area where AI and machine learning are significantly applied is the discovery of new drugs. It’s no wonder that the authors of the groundbreaking AlphaFold 2 model, Demis Hassabis and John Jumper, received the Nobel Prize in Chemistry in 2024 – their work showed how to connect biology, chemistry, and physics with artificial intelligence. AlphaFold 2 can very quickly and accurately predict the three-dimensional structure of proteins from amino acid sequences, which could significantly shorten and perhaps even reduce the cost of developing and testing new drugs.
AI can significantly help with identifying biomarkers that influence treatment response in oncology. For each patient, there is a huge number of variables that affect the final treatment outcome. It’s estimated that half of oncology patients will encounter some type of immunotherapy during treatment. The body’s response is influenced by many factors – the patient’s emotional state, depression, treatment timing, or the presence of immune cells in the tumor. The composition of the microbiome, patient’s BMI, nutrition, and amount of fiber in the diet also play a role. Therefore, it’s not entirely simple to estimate which factors are key in treatment. AI could identify certain patterns in patients that we don’t currently see or register.
Original text: Igor Březina, Roklen 24
